

According to WHO Report, Cardio-Vascular Disease (CVD) are the number 1 cause of death globally: more people die annually from CVDs than from any other cause. An estimated 17.9 million people died from CVDs in 2016, representing 31% of all global deaths. Of these deaths, 85% are due to heart attack and stroke. Over three quarters of CVD deaths take place in low- and middle-income countries. Out of the 17 million premature deaths (under the age of 70) due to noncommunicable diseases in 2015, 82% are in low- and middle-income countries, and 37% are caused by CVDs. Most cardiovascular diseases can be prevented by addressing behavioural risk factors such as tobacco use, unhealthy diet and obesity, physical inactivity and harmful use of alcohol using population-wide strategies. People with cardiovascular disease or who are at high cardiovascular risk (due to the presence of one or more risk factors such as hypertension, diabetes, hyperlipidaemia or already established disease) need early detection and management using counselling and medicines, as appropriate.
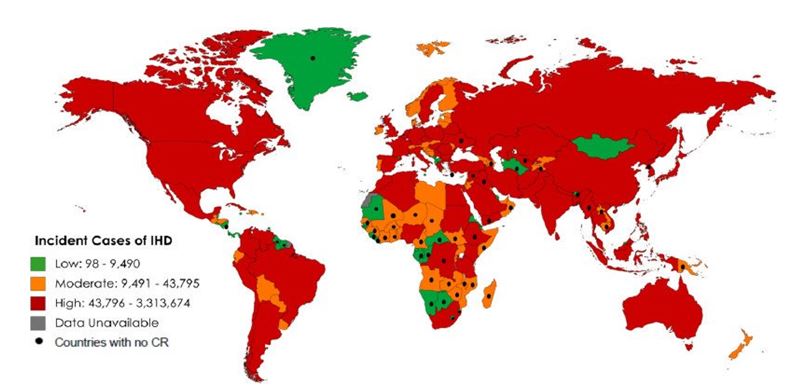
Cardiovascular diseases is a development issue in low- and middle-income countries. At least three quarters of the world's deaths from CVDs occur in low- and middle-income countries. People in low- and middle-income countries often do not have the benefit of integrated primary health care programmes for early detection and treatment of people with risk factors compared to people in high-income countries. People in low- and middle-income countries who suffer from CVDs and other Non-Communicable Diseases (NCDs) have less access to effective and equitable health care services which respond to their needs. As a result, many people in low- and middle-income countries are detected late in the course of the disease and die younger from CVDs and other NCDs, often in their most productive years. The poorest people in low- and middle-income countries are affected most. At the household level, sufficient evidence is emerging to prove that CVDs and other NCDs contribute to poverty due to catastrophic health spending and high out-of-pocket expenditure. At macro-economic level, CVDs place a heavy burden on the economies of low- and middle-income countries. A total-risk approach needs to be adopted for early detection and cost-effective management of hypertension in order to prevent heart attacks, strokes and other complications.
Achieving this target will require strengthening key health system components, including access to health-care technologies and necessary components of medicines and healthcare annexes. The global burden of cardio-vascular mortality is immense. Treatment of the individuals involves hospitalization in which progress reports are maintained manually by nurses and doctors.
Even the calculations of drug dosage depending on the age and gender are done manually and the real-time data such as ECG, ECHO and other investigations and also the heart rate coming from devices connected to the individual is noted manually (on hourly basis by considering only the maximum/average values). These manual entries and calculations have potential to result in high error rate.
In addition, the data produced every second by devices is stored for a maximum of 72 hours and significant quantity of this crucial physiological data may remain unexplored.

i-CCC+ is a cloud-based application that automatizes the workflow of every Cardiology set-up starting from the day of admission till the discharge of the patient, thus reducing the responsibilities of users (nurses, doctors and administrators).
The system comes with screens that are the exact replica of the entire Cardiology workflow like admission form, assessments, progress notes, and nursing charts. In addition, the system captures real-time clinical parameters of every individual coming from multiple devices (which can be viewed on a single interface) and stores variations of the same forever on the cloud, so it can be accessed by the doctor at any point of time. In order to reduce human errors, the system has automatic calculators for ordering/prescribing /monitoring feeds and medication statuses.
It caters to all the responsibilities of various roles/owners (Nurse, Dietician, Rehab. Counselor, Senior Doctor, Cardiologist, and Administrator). It’s an effort to virtually eliminate human error in health monitoring. Solution current USP is in live data monitoring- anytime-anywhere (agnostics to ICCU device vendors), auto discharge summary, and prediction of onset of infections & other perinatal health problems. Post-discharge from the hospital, discharge data is pushed into PHR. The PHR (Patient Health Record) – Automates Vital monitoring, prescription & lab investigations, vaccination record & scheduler.
It also provides the doctors with a solution to all the problems related to manual paperwork (such as duplication of records while preparing progress notes and discharge summary) by automatically generating progress notes of hospital stay as well as a discharge summary.

i-CCC+ leverages IoT integration with biomedical devices in any Cardiology Setup to capture real time vital parameters. These parameters captured by i-CCC amount to millions of data points per day per individual. Stream of data is sent to STATIN layer which stores the same in json and any Structured Database.
The daily datafeed of the patient with multiple parameters are captured in MySQL database. I-CCC+ thus performs the role of the first Big Data hub (of both structured and unstructured data) of individuals across and offering temporal (longitudinal) data of their stay in the Hospital.
This not only allows clinicians to evaluate the efficacy of their interventions, but also provides avenues for translational research. To augment the research purposes, iCCC+ leverages drools based clinical rule based engine and deep learning based big data analytical model coded in R and PMML.
STATIN.BI platform integration with Hospital Information Systems (HIS)
Please contact us with your requirement. We will detail it out and get back to you with the Apps best tailor made to you